Ultrasound imaging allows physicians to directly view nerve damage. Different diseases affect nerves in characteristic ways, some of which can be seen with ultrasound. Ultrasound is well suited for detecting nerve entrapments, such as carpal tunnel syndrome. It is also proving useful for diagnosis and follow-up of inflammatory neuropathies. Read on for more information about nerve ultrasound.
By Einar Wilder-Smith, MD, DTM&H, FAMS, FMH
An important part of medical diagnostics is the ability to visualise directly the nerve damage caused by disease. This is because diseases often affect nerves in specific signature patterns. Recent advances in ultrasound (US) technology have firmly established the value of this diagnostic test for everyday use in the work-up of peripheral nerve disease. Imaging is an ideal complement to the main current diagnostic methods for peripheral nerves, electromyography (EMG) and nerve conduction, which detect nerve function.
A big advantage of US is its excellent tolerability. In contrast, a considerable number of people, and in particular children, cannot tolerate EMG. There is also no need to specially prepare for the testing.
Professional Details
Although US and magnetic resonance imaging (MRI) both depict peripheral nerves well, US is more suited to everyday clinical practice, due to its easy accessibility, superior spatial resolution and low cost. MRI’s main role lies with the imaging of deeper-lying nervous structures and those obscured by bony structures. By revealing nerve size and shape, US anatomically pinpoints peripheral nerve changes and can identify nerve entrapments, trauma, tumors and inflammation.
US is particularly well suited for the detection of nerve entrapments. At the entrapment, the nerve is flattened, in contrast to the swelling occurring just before and after the entrapment (see image). Different locations of nerve entrapment can be diagnosed, ranging from common carpal tunnel syndrome of the wrist, to meralgia paresthetica in the thigh, and rare tarsal tunnel syndrome in the foot.
In addition to the obvious usefulness in the detection of trauma to nerves, US is increasingly helpful in the diagnosis and follow-up of immune neuropathies, including Guillain-Barre syndrome and chronic inflammatory demyelinating polyneuropathy. This is again based on the understanding that different types of nerve inflammation cause different signature patterns of nerve enlargement. Certain genetic causes of neuropathy such as Charcot-Marie-Tooth 1A (CMT-1A) often show massively enlarged peripheral nerves, characteristically outside the typical sites of nerve entrapment, making US a convenient screening method for such conditions.
Most nerve US have a resolution of around 500 µm, enabling imaging of fascicles within nerve trunks in many regions. Commonly scanned nerves include the median, ulnar, radial, peroneal, tibial, sciatic and lateral femoral cutaneous nerve. The cervical nerve roots C5-C6 are readily amenable to US visualization.
A recent expert review summarizes the indications for neuromuscular ultrasound (Walker et al., 2018).
For 2019 reimbursement information, click here.
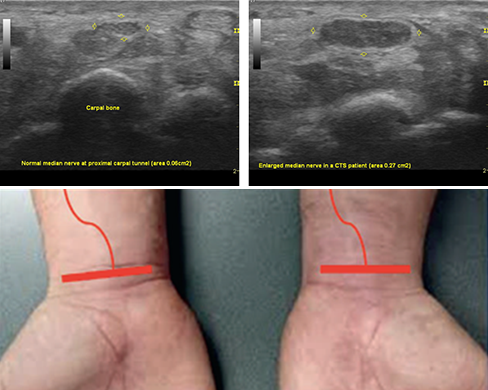
Picturing nerve entrapment: The ultrasound image on the left reveals a normally sized median nerve, marked by yellow arrows, near to the carpal tunnel. In contrast, the technique detects nerve enlargement in a person with carpal tunnel entrapment syndrome (CTS, right panel). Image courtesy of E. Wilder-Smith.
Reference
Indications for neuromuscular ultrasound: Expert opinion and review of the literature.
Walker FO, Cartwright MS, Alter KE, Visser LH, Hobson-Webb LD, Padua L, Strakowski JA, Preston DC, Boon AJ, Axer H, van Alfen N, Tawfik EA, Wilder-Smith E, Yoon JS, Kim BJ, Breiner A, Bland JDP, Grimm A, Zaidman CM.
Clin Neurophysiol. 2018 Sep 25. S1388-2457(18)31234-3.
