Nutritional and Toxic Neuropathies
1. Conditions causing nutritional neuropathies2. Specific nutritional factors:
- B1
- B12
- B6
- Copper
- Vitamin E
3. Toxic neuropathies: heavy metals (mercury), alcohol, medications
4. General considerations regarding work-up and management
Case Study
 54 y/o woman with diabetes, asthma, high blood pressure, morbid obesity (body mass index=65; weight=377 lbs)
54 y/o woman with diabetes, asthma, high blood pressure, morbid obesity (body mass index=65; weight=377 lbs)10/2002: gastric bypass. Post-op had nausea and vomiting with rapid weight loss
5/2003: tingling, numbness in feet, gait imbalance. B12 deficiency suspected (not tested); started intramuscular injections
9/2003: respiratory distress, nausea/vomiting, abdominal pain. Weight=225 lbs.
10/2003: incoordination of hands, numbness, asymmetric limb weakness
X-ray showed enlarged heart and fluid in lungs, leading to insertion of a breathing tube
Risk Factors for Malnutrition
1. Eating disorders (e.g., anorexia, bulimia)2. Limited access (homelessness, low socioeconomic status)
3. Pregnancy-associated vomiting
4. Alcohol abuse
5. Medications: e.g., isoniazid, an antibiotic used to treat tuberculosis→B6 deficiency
6. Malabsorption:
- Intentional (gastric bypass surgery, removal of part of small intestine)
- Medical conditions affecting GI tract: irritable bowel disease, celiac disease, chronic liver/pancreatic disease, stomach irritation and inflammation
Neuropathy After Stomach Reduction Surgery for Treating Obesity
Various forms: bypass, adjustable band, sleeve gastrectomy
Neurologic complications:
Incidence: 0.08-16% found in one study and 4% in another
In review of 50 case reports (96 patients), most common findings were neuropathy (in 62%) and brain disorder (in 31%).
(Koffman et al., Muscle Nerve, 2006)
Risk factors for neuropathy occurring after stomach-altering surgery:- Increased levels of pre-op blood Hemoglobin A1c and triglycerides
- Prolonged nausea/vomiting
- Post-surgical complications
- Rapid weight loss
- Poor follow up at nutritional clinic
- Reduced blood albumin/transferrin levels
(Thaisetthawatkul et al., Muscle Nerve, 2010)
In a controlled study, neuropathy developed in 16% of stomach reduction surgery patients vs. 3% of patients who had gall bladder removal surgery.
Neuropathy subtypes:
- Sensory-predominant: secondary to nutritional deficiencies?
- Mononeuropathy, radiculoplexus neuropathy: more likely in setting of diabetes mellitus?
Immune-mediated cause in some patients?
(Thaisetthawatkul et al., Neurology, 2004)
Specific Nutritional Factors Associated With Neuropathy
- B1 (thiamine)
- B6 (pyridoxine)
- B12
- Copper cause
- Vitamin E
Vitamin B1 (thiamine)
Required for the action of 4 enzymes essential for sugar metabolism
Rapidly depletable (very little stored in body)
Absorbed in small intestine
Sources: whole grains, yogurt, protein foods, nuts, beans, soy
Recommended daily allowance is 1-1.5 mg/day; higher requirements in athletes, pregnancy, cancer
Diagnosis: measure the activity of the enzyme erythrocyte transketolase (better reflects body’s stores) or thiamine pyrophosphate
Treatment of deficiency: 100 mg daily either intravenous or orally
Neurologic signs:
Wernicke encephalopathy: eye changes, balance disturbance, mental confusion
Beriberi (severe deficiency) with/without heart failure (“wet” vs. “dry”)
Neuropathy:
- “Burning foot” syndrome (acute/subacute, predominantly small/large fiber
- sensory)
- Motor-dominant (acute Guillain-Barré Syndrome-like, “dry” beriberi)
- Cranial nerve involvement (weakness of tongue, facial and eye muscles)
B6 deficiency OR excess can cause neuropathy.
Deficiency is rare; usually due to pregnancy/lactation, general malnutrition (e.g., alcoholism), medications (B6 antagonists, e.g., isoniazid, hydralazine, penicillamine, 4-deoxypyridoxine, oral contraceptive pills), chronic dialysis
Sources: fish, beef liver, organ meats, potatoes, starchy vegetables, fruit (other than citrus), fortified cereals
Diagnosis: blood B6 or pyridoxal phosphate levels
Deficiency can cause:
- Painful burning sensations, numbness in feet
- Skin changes
- Seizures (infants)
Treatment for deficiency: <50 mg/day (U.S. RDA=2 mg). Avoid excess!
Neuropathy due to EXCESS B6
Source: homeopathic cold remedies, excess supplementation, energy drinks.
Burning sensations and balance issues described in patients taking 2 grams/day
(Schaumburg et al., N Engl J Med, 1983)
Also reported in patients taking minimum of 200 mg/day
(Parry and Bredesen, Neurology, 1985)
All improved after discontinuing B6
Model of isolated sensory neuropathy without systemic disease
Vitamin B12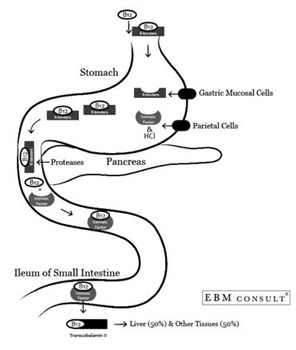
B12: important for myelin sheath (nerve fiber insulation) formation due to
formation of:
1. methionine, tetrahydrofolate;
2. succinyl coenzyme A.
Source: meat/dairy products, fortified foods, supplements
Complex metabolism
Absorbed in terminal ileum
Up to 40% of older adults have low blood B12 levels.
Normal blood values=250-1100 pg/mL; target>400 pg/mL
Vitamin B12 Deficiency
Causes of deficiency:
- Pernicious anemia (immune destruction of intrinsic factor, a protein made in the stomach that is required for B12 absorption. This can cause low red blood cell count with some enlarged red blood cells, which is called megaloblastic anemia.)
- Vegan diet (can take 5 yrs to manifest)
- Medications (proton pump inhibitors, metformin),
- Food-cobalamin malabsorption (due to nitrous oxide exposure [inactivates methyl-cobalamin])
Diagnosis: low B12, elevated methylmalonic acid (MMA) level
Renal disease→false positive MMA elevation
Homocysteine elevation: less specific (also seen with hypothyroidism, folate and vitamin B6 deficiency, advanced age, cigarette smoking)
Additional testing: intrinsic factor and parietal cell antibodies?
Neurologic syndromes associated with B12 deficiency
1. Neuropsychiatric abnormalities
2. Subacute combined degeneration of the spinal cord with involvement of:
- Dorsal columns: loss of sense of position, shown by loss of balance when patient stands with feet together and eyes closed
- Lateral columns: corticospinal weakness (e.g., hip, knee flexors) spastic partial paralysis
- Reflexes: mixed with absent ankle reflexes and brisk knee and ankle reflexes
3. Neuropathy: typically sensory axonal neuropathy +/- damage to spinal cord
- Acute onset, upper +/- lower extremity involvement=clues to diagnosis
- Megaloblastic anemia may NOT be present in patients with neuro manifestations
4. Damage to the nerve to the retina of each eye
B12 deficiency treatment
- Oral: 1000 mcg/day (1%, or 10 mcg; RDA=3-6 mcg/day.)
- Intramuscular injections: 1000 mcg daily X 3-7 days or 1000 mcg weekly X 4, then maintenance with 1000 mcg monthly.
- Intranasal (Nascobal): 500 mcg weekly
Oral as effective as IM?
(Vidal-Alaball et al., Cochrane Database Syst Rev, 2005)
Muscle injection is preferable in pernicious anemia, or with a history of gut malabsorption
Neurologic improvement expected in first 6 months;
May only prevent further neurologic deterioration.
B3 (niacin, nicotinic acid)
Classic clinical triad: skin inflammation, dementia, diarrhea.
Absorbed in intestine via simple diffusion
Risk factors: homelessness, anorexia, certain cancers, malabsorption
Neurologic manifestations: apathy, inattention, irritability, depression.
Not known to be a cause of neuropathy.
Treatment: 50 mg 2-3 times/day.Copper
Component of important enzymes
(e.g., cytochrome C oxidase) for ATP production,
antioxidation, neurotransmitter production,
and cross-linkage of collagen and elastin.
Sources: seafood, nuts, wheat, grains
Absorbed in stomach and proximal duodenum via active or passive mechanisms (depending on dietary levels).
Gastric acid required to solubilize dietary copper.
In liver, copper incorporated into ceruloplasmin for delivery to cells. (Liver excretes excess copper into bile.)
Zinc→upregulation of metallothionein in enterocytes which binds copper→sloughed off in feces.
Copper deficiency→myelopathy or myeloneuropathy
(Kumar et al., Neurology, 2004)
Also hematologic abnormalities: anemia, occasionally myelodysplastic syndrome.
Causes: gastric surgery, excess zinc (supplements or older denture creams), poor diet, clioquinol or idiopathic.
Copper deficiency causing myeloneuropathy (damage to spinal cord as well as peripheral nerves)
Mimics subacute combined degeneration (sensory ataxia due to dorsal column dysfunction, corticospinal tract weakness, lower limb spasticity)
Gait difficulties
Abnormal sensations in skin of lower limb, such as pins and needles, numbness or burning
Dorsal column: loss of position sense, vibration, loss of balance
Lateral column: corticospinal-pattern weakness, spasticity, brisk knee reflexes, extensor plantar responses.
MRI of the spine shows changes in parts of the spinal cord in the neck or thorax in ~50% of cases
(Jaiser & Winston, J Neurol, 2010)
Copper deficiency
Diagnosis: check blood and urine zinc, copper, blood ceruloplasmin.
RDA=900 mcg/day.
Expected values in deficiency:- Low blood copper
- Low ceruloplasmin
- 24-hr urine: low copper (more sensitive than blood level)
- Zinc level in blood/urine: normal or high (if exogenous source)
Treatment: 2 mg elemental copper three times a day
Vitamin E
Alpha-tocopherol=biologically active form of vitamin E in humans, fat-soluble.
Sources: animal fat, vegetable oils, nuts, grains
Incorporated into chylomicrons, passively absorbed in intestines.
Vitamin E delivered to tissues via chylomicrons.
Transferred to very VLDL lipoproteins via alpha-tocopherol transfer protein (TTP).
Deficiency: malabsorption or transport deficiencies (mutations of transfer protein, abetalipoproteinemia), cystic fibrosis.
Pathogenesis: due to loss of protective effect (antioxidant, free radical scavenger).
Neuro manifestations: ataxia, decreased reflexes, loss of sense of position or vibration, speech difficulty, involuntary eye movements, paralysis of eye muscles, damage to the retina, head shaking, decreased sensation and weaknessof muscles in the upper arms and legs.
Nerve conduction studies show sensory-predominant, axonal neuropathy.
Diagnosis: measure blood alpha-tocopherol levels, total blood vitamin E: total blood lipid concentration.
Treatment: 400 IU twice daily, with dose increase until normalization. Higher requirements in abetalipoproteinemia. RDA=15 mg/day
Case Study
 54 y/o woman with diabetes, asthma, high blood pressure, morbid obesity (body mass index=65; weight=377 lbs)
54 y/o woman with diabetes, asthma, high blood pressure, morbid obesity (body mass index=65; weight=377 lbs)10/2002: gastric bypass. Post-op had nausea and vomiting with rapid weight loss
5/2003: tingling, numbness in feet, gait imbalance. B12 deficiency suspected (not tested); started intramuscular injections
9/2003: respiratory distress, nausea/vomiting, abdominal pain. Weight=225 lbs.
10/2003: incoordination of hands, numbness, asymmetric limb weakness
X-ray showed enlarged heart and fluid in lungs, leading to insertion of a breathing tube
Lab studies (October 2003, 2 wks after admission):
B1=0.8 (normal=1.6-4 microg/dL)
B6=2.7 (normal=5-30 ng/mL)
Folate=1 (low)
Anemia of chronic disease
Vitamin E: normal
B12 (=682): normal (receiving IM injections since May 2003).
Spinal fluid protein is twice normal
Electromyogram/nerve conduction studies: axonal sensory and motor polyneuropathy
Diagnosis: Neuropathy due to chronic malnutrition; Guillain-Barre syndrome-like presentation in setting of thiamine deficiency
Toxic neuropathies
Peripheral nervous system: high metabolic rate, vulnerable blood-nerve barrier
Dorsal root ganglia: especially vulnerable (no effective barrier)
Clinical features: neuropathies represented by sensory disturbances
Causes:
1. Alcohol
2. Heavy metals: mercury, arsenic, lead
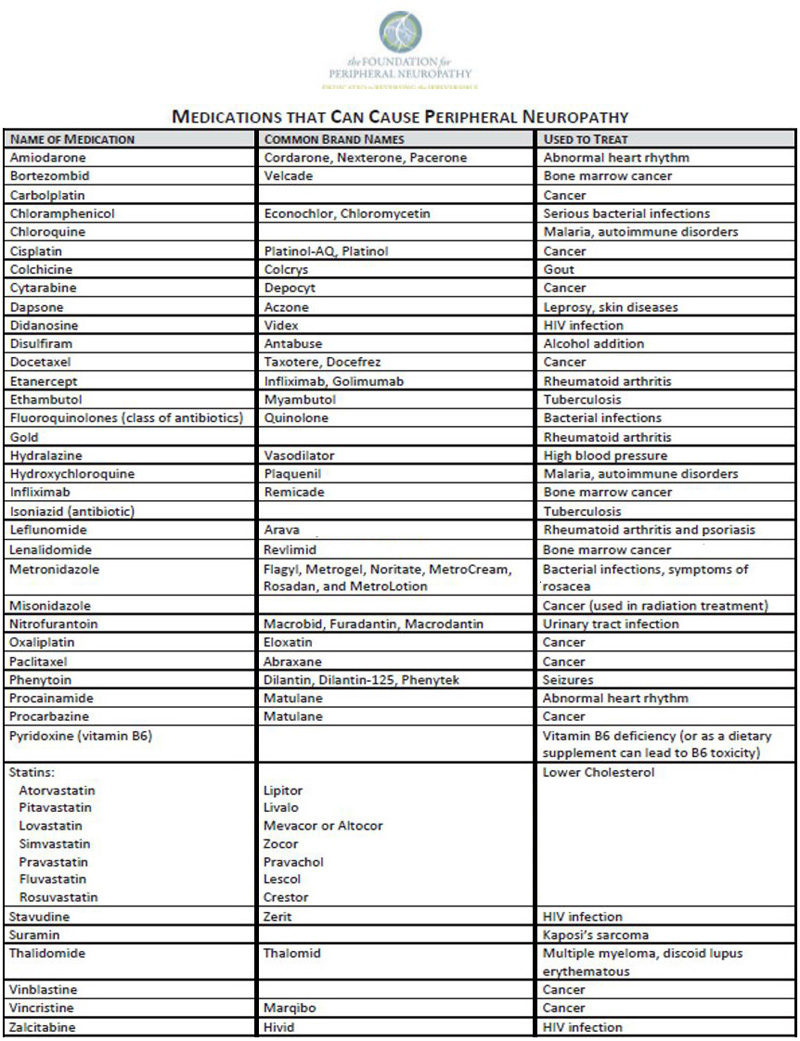
3. Medications: chemo, non-chemo (causal relationship clearly established in minority)Alcohol-related neuropathy
Prevalence (chronic alcoholics): 4-30%
Including those with subclinical neuropathy: 9-67%
Pathogenesis: nutritional deficiency (e.g., thiamine) +/- direct toxic effect, multifactorial
Presentations:
- Painful small fiber, sensory and autonomic dysfunction
- Sensorimotor axonal (numbness, distal weakness, sensory ataxia)
- Acute axonal (Guillain-Barré-like) with normal cerebrospinal fluid protein and more severe sensory symptoms
Mercury toxicity
Effects on nervous system depend on chemical state
Elevated blood methylmercury levels noted in idiopathic axonal neuropathy
Concentration and duration of exposure required for neurotoxicity, response to dietary intervention is unknown.
Larger prospective studies needed.
(Latov et al., JAMA Neurology, 2015)
www.foundationforpn.org
Fluoroquinolones
Peripheral neuropathy: rare but reported side effect.
Food and Drug Administration (2013) included risk of permanent neuropathy as side effect.
Increased risk reported
(Etiman et al., Neurology, 2014)
Statins
Muscle pain (at onset of use) is more typical
Association with peripheral neuropathy more controversial.
Some reports of small fiber sensory/autonomic neuropathy with mild clinical symptoms.
NO association between statins and neuropathy recently reported
(Svendsen et al., Br J Clin Pharmacol, 2017)
Conclusion
In the developed world:
Nutritional neuropathies in setting of inadequate diet, medications, alcohol, malabsorption (GI disease or bariatric surgery).
Toxic neuropathies due to alcohol, medications (chemo, non-chemo), alcohol, heavy metals (mercury?).
Alcohol→thiamine deficiency, direct toxic effect
B6 EXCESS→sensory neuronopathy
B12 deficiency→subacute combined degeneration +/- peripheral neuropathy
Copper deficiency→neuropathy involving nerves of the spinal cord and periphery
These neuropathies are typically length-dependent (affecting lower legs and arms), sensory or sensorimotor, axonal.
Repletion of deficiency or elimination of toxin may arrest progression, but recovery may be limited.
